Contents
Humans have 5 senses: touch, taste, smell, sight, and hearing. The senses are based on receptor cells or groups of receptor cells called sense organs.
Receptors respond to stimuli and send nerve impulses along sensory neurons. (See nervous system page) The brain interprets the nerve impulse and, thus, we perceive the impulse as one of our senses.
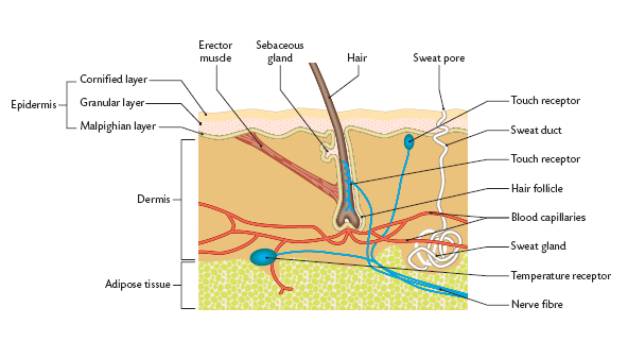
Touch
The skin is the organ, which contains the receptors for touch and temperature. The skin was discussed extensively in the excretion page. The receptors are found in different concentrations at different areas of the body. An example is that there are few touch receptors at the heal of the foot but many temperature receptors at the elbow.
Taste
Receptors for taste are located on the tongue at the taste buds. The taste buds are at the top and the sides of the tongue. (See diagram below) Some taste buds are also found in the lining of the throat.
Note that there are 4 different taste receptors: sweet, sour, salt, and bitter. Note that the different types are located at different areas of the tongue.

The sense of taste is a combination of taste as well as smell, texture, and temperature. Cold food tastes different than hot food. If you squeeze your nostrils closed when you eat you will not taste the food as strongly. Also, if you have a cold your sense of taste is diminished. We continue to taste some foods after we eat them because bits of the food become lodged on out tongues and the taste receptors are still sending impulses as a result.
Sight
Sight is, of course, the function of the eye. It is very important that you know the parts of the eye and the functions of the parts of the eye.
Sclera: tough outer white layer of the wall of the eye. It along with internal fluid pressure keeps the eyes shape and protects its delicate internal parts.
Conjunctiva: is a thin, clear membrane covering the front of the eye and inner eyelids. Cells in this lining produce mucous that helps to lubricate the eye. This is the eyes first layer of protection against infection. Inflammation of this membrane is called conjunctivitis, or pink eye.
Cornea: transparent ‘window’ of the eye, focussing of light on the retina. It is the first and most powerful lens in the eye’s optical system. To keep it transparent the cornea contains no blood vessels. Tears that flow over it and aqueous humor in the chamber behind it keep it nourished. When you hear of eye banks and eye transplants, it is the cornea that is being replaced. The cornea can be damaged from: accidents, infections, and genetic defects. The cornea bends the light toward the retina.
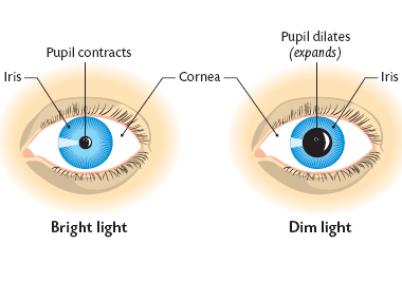
Iris: the coloured ring of muscle fibers located behind the cornea and in front of the lens. It contracts andexpands, opening and closing the pupil, in response to the brightness of surrounding light. Just as the aperture in a camera protects the film from over exposure, the iris of the eye helps protect the sensitive retina. Melanin is the pigment that produces dark eyes. Blue eyed people have no melanin in their iris.
Pupil: a hole in the iris letting light into the back of the eye. The iris muscles control its size. (See discussion of pupil below)
Ciliary Body: a ring of muscle controlling the shape of the lens.
Suspensory Ligaments: transfer the pull of the ciliary body to the lens.
Lens: controls the fine adjustment to the focussing of light onto the retina. It is an elastic transparent structure. It changes shape to focus light onto the retina.
Retina: light sensitive layer of rods and cones converting light into nerve impulses. The retina is the film of the eye. It converts light rays into electrical signals and sends them to the brain through the optic nerve. The sides of the retina are responsible for our peripheral vision. The center area, called the macula, is used for our fine central vision and color vision. (See discussion of rods and cones below)
Fovea or Yellow Spot: a tiny area of densely packed cones for detailed and coloured vision. It contains only cones. This small part of our retina is responsible for our highest visual acuity. It is the centre of our central vision.
Choroid: a black-pigmented layer preventing internal reflection of light. The choroid is a layer of blood vessels between the retina and sclera; it supplies blood to the retina.
Blind Spot: exit point of the optic nerve cutting through the retina so no rods or cones here.
Optic Nerve: carries the impulses from the rods and cones to the visual centre of the brain. Each optic nerve has about 1.2 million nerve fibers. This is the cable connecting the eye to the brain.
Aqueous Humour: a clear liquid in front of the lens maintaining the shape of the cornea. A water like fluid, produced by the ciliary body, it fills the front of the eye between the lens and cornea and provides the cornea and lens with oxygen and nutrients. It drains back into the blood stream through the canals of schlemm.
Vitreous Humour: a clear jelly offering support and shape to the back of the eye. The vitreous humor is a jelly like liquid that fills most of the eye (from the lens back). As we age it changes from a gel to a liquid and gradually shrinks separating from the retina. This is when people start seeing floaters, dark specs in their vision. This is a normal sign of aging, but in a few cases the retina can become detached as the vitreous separates.
External muscle: The eye is moved by 6 external muscles.
Rods and Cones

Cones (left) are receptors responsible for colour and rods (right) receive black and white.
Cone cells function in bright light and are responsible for colour vision. The 6 million cones in each eyeball are sensitive to colour rather than lightness and are concentrated towards the centre of the retina where there is more light. Each cone contains photopigments that are attuned to a particular band of the spectrum. When they detect light within their range they produce an electrochemical response. In humans there are three main sorts of cone, which respond to either long, medium or short wavelengths. They’re usually called red, green or blue cones because these are the predominant colours within each band. However, the spectral bands they detect are actually quite wide and overlap each other. Other animals have a smaller or greater number of different cones. Many animals also have cones capable of detecting ultraviolet light. Cones require a reasonable amount of light to be stimulated so only function during the day. This is why we have better colour vision during the daytime when the light intensity is high enough to stimulate the cone receptors.
Rod cells are able to function in dim light but do not perceive colour. Each eye has about 120 million rods, which tend to be concentrated more around the outer edges of the retina. Rod cells are able to work in low light intensity because the cell can respond to a single photon of light (more sensitive). The brain requires fewer than 10 such responses to perceive the sensation of a flash of light. Rod cells however are unable to distinguish colour therefore despite being more sensitive than cones to light they enable us to see at night but only in black and white.
Diagram showing the inside of the eye and a small section of the retina. The eye diagram shows the lens in the front of the eye and the retina and optic nerve opposite it at the back of the eye. The section of the retina illustrates the rods and cones and shows how they are linked to the optic nerve.
The Pupil
The pupil is the opening of the eye. Through this opening light enters the eye. The size of the opening is determined by the amount of light present. The size of the pupil becomes smaller (contracts) as the iris become larger. The size of the pupil becomes larger (dilates) as the iris becomes smaller. So, the size of the iris determines the size of the pupil. The change in the size of the iris is a reflex action carried out in response to the light intensity.
Common Problems of Sight
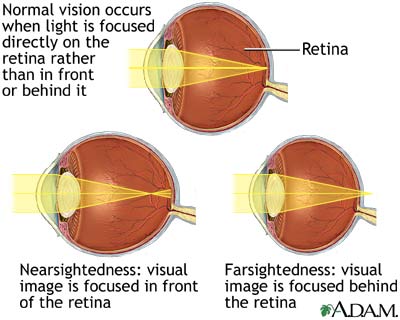
Figure 2: If you are nearsighted, the image comes into focus before it hits your retina (top). A concave lens can push the focus back (bottom).
Here are the four common refractive vision problems:
Nearsightedness (myopia)
Farsightedness (hyperopia)
Astigmatism
Presbyopia
In nearsightedness (myopia), the light from distant objects gets focused in front of the retina rather than on it. Myopia happens usually when the eyeball is too long; however, it is sometimes caused by too much focusing power in the lens system. See Figure 2. The result is that the person can see close-up objects fine, but distant objects are blurry. Myopia can be corrected by using a concave lens to diverge, or spread out, the light so that when it passes through the lens system, it comes to focus on the retina.
Figure 3: If you are farsighted, the image doesn’t come into focus before it hits your retina (top). A convex lens can bring the focus forward (bottom).
In farsightedness (hyperopia), the light gets focused in back of the retina rather than on it. See Figure 3. Hyperopia usually happens when the eyeball is too short or when the focusing power of the lens system is too weak. The result is that a person can see distant objects fine, but close-up objects are blurry. Hyperopia can by corrected by using a convex lens to concentrate or converge the light (Figure 3) so that when it passes through the lens system, it comes to focus on the retina.
To Review:
Normal, near, and farsightedness:
Note: you have a choice – correction of long and short sight or correction for a hearing defect.
In astigmatism, the shape of the cornea or the lens is distorted so that the light comes into two focal points. Imagine that the lens is egg-shaped instead of spherical and that light coming over the top and bottom edges is brought to a different focal point than light coming over the right and left sides. To correct this problem, a lens that is shaped to correct the distorted shape of the eye’s lens system is made.
In presbyopia, the cornea and lens of the eye become less stretchy and, therefore, they cannot change shape as readily to bring light to a focus on the retina; this happens naturally as we grow older and is usually observed when a person reaches their 40s. If you have presbyopia, you have trouble focusing light from both near and far objects on the retina. To correct this problem, you might get a pair of bifocal lenses, with the top part for seeing far objects and the bottom part for near objects.
Hearing
The ear is the organ for hearing and balance. In hearing the ear detects vibrations, their frequency (pitch) and amplitude (loudness). These become nerve impulses carried to the brain. For balance the ear detects the direction of motion, acceleration and head position related to gravity.
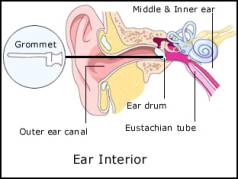
There are 3 sections to the ears: the outer ear, the middle ear, and the inner ear. See the diagram below for the parts of the ear. It is very important that you know these parts and their functions.
Middle Ear:
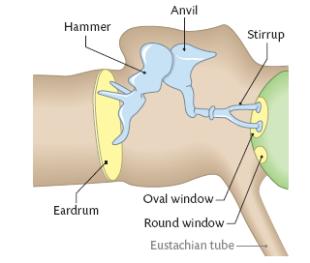
Pinna: Is said to collect sound waves and channel them into the external auditory canal. It is made of mainly of cartilage.
Auditory Canal: This is the tube that carries sound vibrations to the eardrum. Earwax and hairs prevent foreign material entering the ear.
Eardrum (tympanum): It is a small, tightly stretched membrane that separates the outer ear from the middle ear. It vibrates with the same frequency as the sound waves beating against it.
Ear Ossicles (hammer, anvil, stirrup): These are three tiny bones in the middle ear. They transmit and amplify the vibrations of the eardrum to the inner ear.
Eustachian Tube: This is a tube that runs from the middle ear to the pharynx (throat). When it opens it equalises the air pressure on both sides of the eardrum allowing the eardrum to vibrate freely so accurate sound sensations are generated. This also prevents damage to the eardrum caused by differences in air pressure between the outer and middle ear.
Oval Window: This is a flexible partition allowing transfer of vibrations from the middle ear to the inner ear.
Round Window: This is a flexible partition to deaden the pressure changes in the inner ear. It allows the pressure waves to dissipate out of the cochlea into the air of the middle ear.
Cochlea: This is responsible for the conversion of sound waves into nerve impulses. (See discussion of how we hear below)
Auditory Nerve: This is the nerve that carries impulses from the cochlea to the brain’s hearing centre.
Semicircular Canals: These detect the direction of motion and acceleration. They are responsible for balance. (See discussion of balance below)
How We Hear
When sound waves enter the ear they vibrate the eardrum. The eardrum causes the ear ossicles (hammer, anvil, stirrup) to move (vibrate). These vibrations arrive at the cochlea. Within the cochlea is a liquid called lymph. The lymph is moved within the cochlea. This movement of liquid stimulates sensory (sound) receptors in the cochlea. There are about 24,000 sensory cells within our ears. These receptors create an electrical impulse that travels up the auditory nerve and on to our brain.
Animations of normal hearing:
Sound waves are first collected in our outer ear (called the auricle or pinna), pass through our ear canal and cause our eardrum to vibrate. These vibrations are in turn transmitted to our inner ear by the bones of our middle ear. Our inner ear plays a vital role in the transformation of these mechanical vibrations into electrical impulses, or signals, which can be recognized and decoded by our brain. When the vibrations reach the cochlea through movement of the bones in the middle ear, the fluid within it begins to move, resulting in back and forth motion of tiny hairs (sensory receptors) lining the cochlea. This motion results in the hair cells sending a signal along the auditory nerve to the brain. Our brain receives these impulses in its hearing centres and interprets them as a type of sound.
Sound waves are vibrations of air particles. As these vibrations strike the outer ear, the Pinna (a) funnels and amplifies them, sending them down the ear canal. At the end of the ear canal (b), the vibrations move the eardrum (c) that in turn vibrates the 3 smallest bones in the body. The Hammer, Anvil and Stirrup (d) further increase the power of the sound and transmit the energy to the inner ear organ of hearing, the cochlea (e) which converts the vibrations to nerve impulses which move to the brain along the auditory nerve (f).
Balance
Balance is controlled by the vestibular apparatus in the inner ear. It consists of the 3 semicircular canals.
The vestibular apparatus is filled with the liquid called lymph. Receptors within the apparatus detect whether the head is vertical or not. Other receptors detect motion. These receptors send impulses to the brain.
Smell
The olfactory region is high up in the nasal cavity. It contains about 20 million neurons that detect odours. They are called olfactory neurons. These neurons send impulses when they dare stimulated by gases. The responses produced by these stimuli can produce about 10,000 different smells. The receptors stop sending stimuli very quickly. That is why we get used to smells very easily.
Middle Ear Infection-Otitis Media
Otitis media refers to inflammation in the middle ear area. There are different forms of otitis media. Typically, when the doctor refers to an ear infection, he or she is most likely talking about “acute otitis media” (although there’s also the common ear infection called swimmer’s ear, or otitis externa).
Acute otitis media is the presence of fluid, typically pus, in the middle ear with symptoms of pain, redness of the eardrum, and possible fever.
Other forms of otitis media are either more chronic in nature (meaning that there’s fluid in the middle ear for 6 or more weeks) or there’s fluid in the middle ear that’s temporary and isn’t necessarily infected (this is called otitis media with effusion).
The reason that doctors try to distinguish between the different forms of otitis is because it affects treatment options. Not all forms of otitis need to be treated with antibiotics.
Causes
Children develop ear infections more frequently in the first 2 to 4 years of life for several reasons:
Their eustachian tubes are shorter and more horizontal than those of adults, which allows bacteria and viruses to find their way into the middle ear more easily. Their tubes are also narrower and less stiff, which makes them more prone to blockage.
The adenoids, which are gland-like structures located in the back of the upper throat near the eustachian tubes, are large in children and can interfere with the opening of the eustachian tubes.
Children’s immune systems aren’t fully developed until the age of 7. Therefore, they have more trouble fighting infections.
There are also a number of other factors that contribute to children getting ear infections. The more common ones are exposure to cigarette smoke, bottle-feeding, and day-care attendance.
Ear infections also occur more commonly in boys than girls, in children whose families have a history of ear infections, and more often in the winter season when upper respiratory tract infections or colds are most frequent.
Signs and Symptoms
The signs and symptoms of acute otitis media may range from very mild to severe:
The fluid in the middle ear may push on the eardrum, causing ear pain. An older child may complain of an earache, but a younger child may tug at the ear or simply act irritable and cry more than usual.
Lying down, chewing, and sucking can also cause painful pressure changes in the middle ear, so a child may eat less than the normal amount or have trouble sleeping.
If the pressure from the fluid build-up is high enough, it can cause the eardrum to rupture, resulting in drainage of fluid from the ear. This releases the pressure behind the eardrum, usually bringing on relief from the pain.
Fluid build-up in the middle ear also blocks sound, which can lead to temporary hearing difficulties. A child may:
not respond to soft sounds
turn up the television or radio
talk louder
appear to be inattentive at school
Other symptoms of acute otitis media may also include:
fever
nausea
vomiting
dizziness
However, otitis media with effusion often has no symptoms at all. In some children, the fluid that’s in the middle ear may create a sensation of ear fullness or “popping.” As with acute otitis media, the fluid behind the eardrum can block sound, so mild temporary hearing loss can happen, but it may not be obvious.
Ear infections are also frequently associated with upper respiratory tract infections and, therefore, with their common signs and symptoms, such as a runny or stuffy nose or a cough.
Diagnosis and Treatment
If you suspect that your child has an ear infection, he or she will need to visit the doctor, who should be able to make a diagnosis by taking a medical history and doing a physical exam.
To examine the ear, doctors use an otoscope, a small instrument similar to a flashlight, through which they can see the eardrum.
There’s no single best approach for treating all middle ear infections. In deciding how to manage your child’s ear infection, a doctor will consider many factors, including:
the type and severity of the ear infection
how often your child has ear infections
how long this infection has lasted
how old your child is
risk factors your child may have
whether the infection affects your child’s hearing
The parents’ wishes are also factored in to this decision, so an open line of communication between you and the doctor is very important.
The fact that most ear infections can clear on their own has led a number of physician associations to recommend a “wait-and-see” approach, which involves giving the child pain relief without antibiotics for a few days. There are other important reasons to consider this type of approach.
Antibiotics:
won’t help an infection caused by a virus
won’t eliminate middle ear fluid
may cause side effects
typically do not relieve pain in the first 24 hours and they have only a minimal effect on pain after that
Also, frequent use of antibiotics can lead to the development of antibiotic-resistant bacteria, which can be much more difficult to treat.
However, children who get a lot of ear infections may be prescribed daily antibiotics by their doctor to help prevent future infections. And younger children or those with more severe illness may require antibiotics right from the start.
The “wait-and-see” approach also might not apply to children with other concerns, such as cleft palate, genetic conditions such as Down syndrome, underlying illnesses such as immune system disorders, or a history of recurrent acute otitis media.
Children with persistent otitis media with effusion (lasting longer than 3 months) should be re-examined periodically (every 3 to 6 months) by their doctors. Often, though, even these children won’t require treatment.
Whether or not the choice is made to treat with antibiotics, you can help to reduce the discomfort from your child’s ear infection by using acetaminophen or ibuprofen (which you can buy over the counter at your local pharmacy or grocery store) for pain and fever as needed. Your child’s doctor may also recommend using pain-relieving eardrops, as long as the eardrum hasn’t ruptured.
But certain children, such as those with persistent hearing loss or speech delay, may require ear tube surgery. In some cases, an ear, nose, and throat doctor will suggest surgically inserting tubes (called tympanostomy tubes) in the tympanic membrane. This allows fluid to drain from the middle ear and helps equalize the pressure in the ear because the eustachian tube is unable to.
Prevention
Although certain factors associated with the development of ear infections can’t be changed (such as family history of frequent ear infections), there are certain lifestyle choices that can minimize the risk of children developing ear infections:
breastfeeding infants for at least 6 months, which helps to prevent the development of early episodes of ear infections. If a child is bottle-fed, holding the infant at an angle rather than allowing the child to lie down with the bottle is best.
avoiding exposure to second-hand tobacco smoke, which can increase the frequency and severity of ear infections.
reducing exposure, if possible, to large groups of children, such as in child-care centres. Because multiple upper respiratory infections may also lead to frequent ear infections, limiting exposure to large groups of kids may result in less frequent colds early on and, therefore, fewer ear infections.
hand washing for both parents and children. This is one of the most important methods of decreasing person-to-person transmission of the germs that can cause colds and, therefore, ear infections.
keeping children’s immunizations up-to-date, because certain vaccines can help prevent ear infections.
Glue Ear and Grommets
Grommets – A grommet is a small, dumbbell-shaped plastic tube, which is slipped through a tiny incision in the eardrum of a child. The surgical insertion of grommets is one of the most common childhood operations in Ireland.
Why is it performed?
Grommets may be inserted if a child has a history of repeated severe ear infections. However they are mainly used in the treatment of a condition known as glue ear, which is a very common problem in children and can cause deafness.
Glue ear occurs when the glue or fluid accumulates in the middle ear, clogging up the hearing mechanism. The glue accumulates due to a blockage of the Eustachian tube, which connects the middle ear and the back of the throat. When inserted, the grommet acts as a pressure equalisation tube for the child, providing a temporary, extra Eustachian tube and allowing bacteria and fluid to drain from the middle ear.
Grommets have been widely used in Ireland since the 1950s. The surgical procedure to insert them is simple and safe and ill effects are extremely rare. Once inserted, the child is usually completely unaware of their presence.
Grommets will then usually fall out of their own accord after a number of months. The child is usually unaware that this has even happened. If they do not fall out spontaneously within 18 months, they will be removed by the ENT surgeon in a simple and painless procedure. The tiny hole left in the eardrum after the removal of grommets will then heal itself.